Let's connect
Tell us how we can help, and a Maximus Canada team member will contact you as soon as possible. Remember, any information you share is protected by our Privacy Statement.

Transform health administration with intelligent automation, efficient workflows, and cost-effective infrastructure.
Medigent® is the leading cloud-based solution for health administration automation.
Government health programs use Medigent to automate claims, streamline enrolment and program eligibility, and share data within their jurisdiction. With a connected view of the beneficiary journey, you can focus on driving value for beneficiaries, while significantly reducing your administrative workload.
Designed to automate health programs at scale, Medigent is a perfect fit to modernize legacy systems worldwide.

The latest version of Medigent is delivered as a secure, SaaS-based cloud service. This ensures rapid deployment, scalability, and ongoing innovation for health programs, including emerging AI and machine learning technologies.
Medigent supports FHIR and HL7 standards for secure, efficient data exchange across diverse systems, fostering healthcare collaboration and seamless interoperability.
As a cloud-service, Medigent is also flexible and scalable, to meet the growing demands of modern health systems.
Enhanced security and compliance through Microsoft Azure provides built-in enterprise-grade security, compliance with global standards (e.g., HIPAA, PIPEDA, GDPR) and continuous updates to maintain a secure environment.
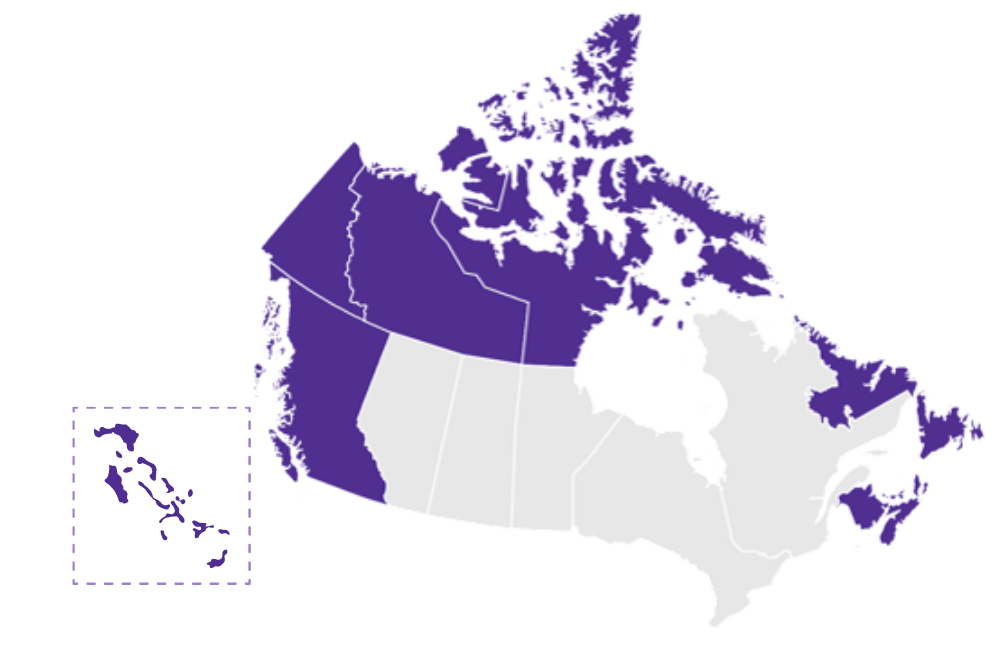
Medigent is trusted by 9 provinces and territories across Canada, the self-governing Territory of Nunatsiavut, and the nation of The Bahamas.
Let’s talk about your health program. How can Medigent help?
Tell us how we can help, and a Maximus Canada team member will contact you as soon as possible. Remember, any information you share is protected by our Privacy Statement.
Where do you need to grow? Medigent supports your health care system with flexible modules that can be deployed independently or in any combination, with the option to scale and add modules as program requirements evolve.
Across Medigent modules, integrated communications and task management tools also improve productivity for users:
Medigent Claims Processing Solutions put powerful automation and smart business rules at the heart of your operations. Whether you’re modernizing all benefit programs at once or taking an incremental approach, Medigent adapts to your needs. Advanced rule configuration means your team can focus on priority claims and better service–while routine assessments are handled automatically.

Take the complexity out of physician and hospital claims.
Medigent’s Medical module is built to handle the full spectrum of payment models and integrates seamlessly with your financial systems. With configurable rules and support for ICD9 and ICD10 standards, manual adjudication becomes the exception, not the rule.
What you can do:
The Pharmacy and Supplementary Benefits module automates and streamlines daily business processes for drug insurance programs. It manages end-to-end Prior Authorization workflows and supports CPhA 3.0 and NeCST messaging for online pharmacy claims. Medigent also enables real-time claims through integration with a vendor’s point of sale software, by batch processing, or manual entry.
Medigent’s Dental module gives you the power to improve dental claim processing through real-time and batch adjudication that integrates business and financial rules. Dental offices across Canada can submit claims electronically, while trial adjudications and policy enforcement keep everything running smoothly.
Flexible fee code structures allow you to set age, frequency, and fiscal controls, ensuring your policies are always enforced. In Canada, the Medigent Dental module is fully CDAnet compliant. Internationally Medigent can adapt to any EDI standard including DentalXChange, NHSBSA, Dentally, HICAPS, etc.
Medigent’s Medical Transportation module gives you control over costs associated with a client’s medical transportation. Pre-authorize, track, and reconcile every aspect of a client’s medical journey - from departure to return. From air and ferry to ambulance, medivac and accommodations, you can automate information capture with electronic loading from third-party systems.
For complete transparency, Medigent lets you link vendor invoices to pre-authorizations, record payments, subsidies, and credits. These tools also give you new insights to flag unauthorized travel. Plus, integration with your financial systems ensures payments are accurate and timely.
For the traveller and any escort, Medigent supports vouchers, uploading and managing receipts, and access to review claim status. This allows for quick repayment while reducing email and phone call volumes.
The portal also allows for direct, secure and tracked communication between the eligible beneficiary and the health jurisdiction.
Medigent’s reciprocal billing capabilities allow you to manage the complete lifecycle of claims associated with inter-jurisdictional reciprocal agreements.
Within the Medical module, Medigent handles claims adjudication and payment processes associated with the Medicare reciprocal program, where programs and adjudication rules vary according to the policies of each jurisdiction.
Medigent adapts to each jurisdiction’s policies and rules. For out-of-province beneficiaries, Medigent supports in-province claims for hospitals and physicians. In-province beneficiaries are also supported for any out-of-province hospital and physician claims.
Capabilities include invoice management, claims processing, adjustment requests, recoveries, and payment processing.
These capabilities can also be leveraged for processing invoices associated with non-reciprocal reimbursements such as out-of-country claims from residents.
Connect eligible residents with the health programs they need, with confidence that only those who qualify are enrolled. Medigent makes it easy to register clients, determine eligibility, and assign benefit plans.

A full set of point-of-service beneficiary management functions, combined with workflow automation, help you manage client information and eligibility, health card services, and client communications.
Module Features:
Synchronize this module with an existing database, or use it as a stand-alone client registry system.
Give providers the tools they need to spend less time in admin – and more time serving patients.
Medigent’s Provider Portal supports digital services and secure self-service for registered practitioners and health care administrators.
With Medigent, registered providers and authorized users can:
The Provider Portal’s user interface is designed for any industry-standard web browser, so providers and authorized support staff will be able to access self-serve functions using their computer or mobile devices such as smart phones and tablets.
The Medigent® Drug Information System gives pharmacists, physicians, and other healthcare providers a connected, real-time view of patient medication records.

The Medigent Drug Information System is the first of its kind in Canada, and compliant with both the FHIR and HL7v3 messaging standards. It enables secure e-prescribing and supports integration with pharmacies, clinics, and hospitals.
Providers can quickly identify potential drug interactions, allergies, and immunizations, helping to prevent harmful errors and improve patient safety.
The system also offers a searchable drug knowledge base and tools for pharmacists to monitor dispensing issues, ensuring residents receive the safest and most effective care possible.
The Medigent Drug Information System helps pharmacists, practitioners and other service providers make informed decisions about patient care. Health care providers can:
Download our smart sheet to learn more about Medigent.

Smart sheet: Medigent
Download the PDFWhy Medigent?
As the market-leading health administration solution, Medigent enables you to find new efficiencies in your health program. With a connected view of the beneficiary journey, detailed analytics, and KPIs, you have the insight to make evidence-based decisions that power streamlined operations and ROI.
Over 95 percent of claims are automated, and continuous innovation ensures a complete view of the beneficiary journey. With Medigent, you transform health care administration to achieve better value for your beneficiaries and programs.
Medigent is not only the leading health administration platform for Canadian provinces and territories – it’s also making an impact internationally. The National Health Insurance Authority of The Bahamas uses Medigent to automate workflows, improve accuracy, and reduce administrative effort. These enhancements have helped The Bahamas modernize their health system, safeguard program rules, and streamline administration.

As public sector healthcare organizations navigate mounting pressures – from capacity and funding constraints to evolving patient needs – health process automation offers a transformative path forward. Medigent enables jurisdictions to invest in healthcare funding where it matters most: serving the citizen.Alain Tremblay National Vice President, Product Division